Following an injury, enhancing, and optimising the recovery process, is a primary concern for anyone who likes to move and feel healthy. Additionally, preventing injury is even better! Conventional treatments of rest, immobilisation, ice etc. are well known. This article considers the role of nutrition in enhancing the recovery of connective tissue, foods and supplements that may aid the process and a list of non-nutrition factors that may a play a role in prevention and recovery.
What is connective tissue?
Connective tissue is a group of tissues (made up of cells) that maintain the structure of the body and its organs, providing a structural and functional role. Examples of connective tissue include: bone, cartilage, ligaments, tendons, muscles, fascia and blood.
Nutrition can play a key role in connective tissue repair and looking at both the nutrients that help the injured connective tissue repair and how to increase blood flow to the tissue is all part of the healing process. Below I am going to list foods that can aid tendon and ligament health and also list supplements I would recommend during acute injury and perhaps for maintenance.
Can nutrition help connective tissue injury recovery?
Below are the key phases of injury recovery with possible roles of nutrition to support the process.
1.Inflammation and immobilisation
A natural and healing response to injury is an inflammatory response. The length of this stage may last from hours to several days, depending upon the type and severity of the injury and usually requires immobilisation. This is likely to result in functional changes, such as loss of muscle strength, as well as metabolic changes in surrounding soft tissue, such as tendons and ligaments.
The role of nutrition: whilst the inflammatory response is important and necessary, nutrients that can prevent excessive inflammation may theoretically be helpful.
2. Rehabilitation and increased activity of injured area
This phase usually includes a progressive return of mobility, consolidation of the healing process (such as the repair of tendons, healing of fractures), regeneration of muscle tissue and a gradual development of muscle strength and size.
The role of nutrition: specific nutrients that may aid the process of repair for tendons, ligaments, cartilage and facilitate the connection to bone/muscle may theoretically be helpful. As well as nutrients that aid the synthesis of muscle tissue may also be helpful.
Can nutrition help connective tissue inflammation?
Omega-3s:
A growing amount of research indicates the role of omega-3 polyunsaturated fats (EPA and DHA) to have anti-inflammatory actions (1). Whilst the appropriate dose to elicit an anti-inflammatory effect in humans is unclear, in the initial stages following an injury, increasing omega-3 intake and decreasing omega-6 intake is likely a helpful strategy to manage levels of inflammation.
Supplementation with EPA and DHA and consuming more fatty fish such as salmon, trout, mackerel and sardines, as well as flax, walnuts and pumpkins may be helpful. Additionally decreasing intake of omega-6 fats, that are mostly found in processed foods and vegetable oils such as corn and sunflower oil.
Protein intake:
Increasing protein intake to adequately facilitate the process of muscle protein synthesis at rest and is necessary during immobilisation – shooting for 2-2.5 grams of protein per kg of bodyweight a day is recommended (2). However, this should be adapted to your optimal bodyweight should your body fat levels be higher than optimal.
Protein quality:
The anabolic effects of protein or amino acids (the building blocks of protein) is blunted during prolonged periods of inactivity and therefore considering protein quality may be helpful. Research shows the benefits of leucine-rich protein sources for stimulating muscle protein synthesis, so considering a leucine rich protein supplementation such as whey, or if plant-based, added leucine, may be advisable.
Steve has formulated a plant-based recovery protein powder which includes organic pea and rice protein, added leucine, creatine, magnesium and organic cacao and can be used to make smoothies, pancakes, oat bowls, yoghurt pots etc. For more information, check out PFORM Restore.
Energy intake
The size of any decrease in energy output during the immobilisation period is likely not as great as expected since the process of healing may increase energy expenditure from 15-50% dependent upon type and severity of injury. Muscle protein synthesis is energetically expensive. If energy restriction is too great then recovery will be slowed, it will be detrimental to healing and exacerbate muscle loss.
Therefore, striking the appropriate balance of energy is key for optimal healing and recovery.
Can nutrition support the connective tissue rehabilitation phase of injury recovery?
Protein intake:
Again, meeting daily protein intake is a priority in order to maximise the process of developing muscle strength and size during rehab – 2-2.5 g/kg/day is recommended (2). Consider working with a Nutritionist to help calculate specifics and plan out meals and foods to aid recovery.
Protein quality:
Again, opting for high quality protein – so either whey or a rice/pea blend with added leucine may aid muscle protein synthesis rates and therefore aid the process of rehab.
Energy intake:
Since total energy expenditure will increase as activity levels increase, increasing energy intake accordingly to support this is necessary. Additionally, sufficient energy availability is crucial to support bone health and reduce fracture risk.
Carbohydrate:
Carbohydrate availability is an important part of total energy intake since carbohydrates are the most readily used source of fuel to generate energy and can help contribute to an anabolic environment conducive to muscle growth and repair.
Nutrient timing
Since there is a maximum amount of protein that can be utilised for muscle protein synthesis at one time (approx. 20-30g), it would be advisable to distribute total protein intake relatively evenly between meal opportunities – for example 4-5 times throughout the day.
Creatine:
Supplementation has been shown to reduce loss of strength and mass during immobilisation (3). Creatine can be found naturally in red meats and can also be supplemented.
Steve included this as part of PFORM Restore to aid overall recovery from training and as a way to support injury recovery and rehabilitation.
Do nutrients help with connective tissue health and recovery?
Relatively little is known about tendon biology and healing and whilst there is logic about the role of these micronutrients in supporting tendon and soft tissue growth, regeneration, recovery, and repair, in practise, the research is limited. The following nutrients either have definite logic behind ensuring that they are well supplied within the diet, or the nutrient is supported by robust research to indicate its role in the enhancing the healing and recovery process.
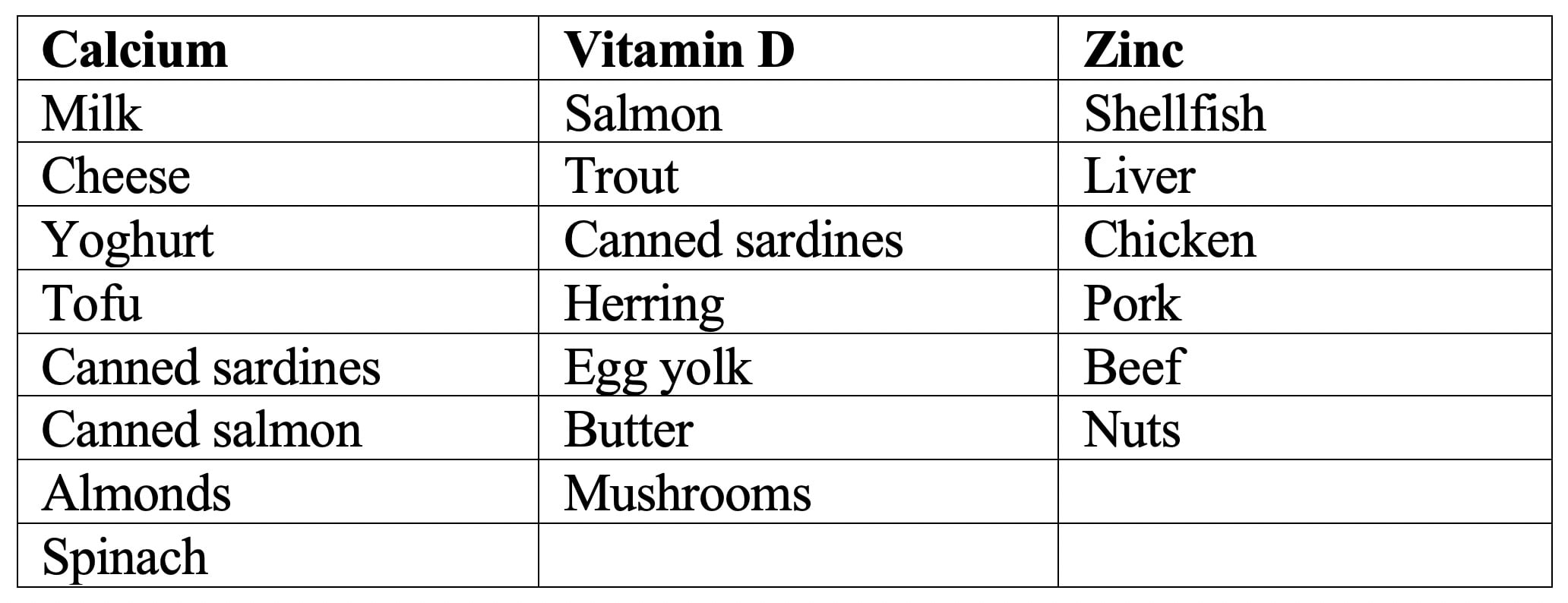
Zinc: is crucial for numerous processes associated with protein turnover – integral to the health of all connective tissue. Zinc activates critical substances which are involved in the development, growth and remodelling of connective tissue. It is well known that insufficient zinc impairs wound healing in hospital patients following injury/surgery (4) and that zinc plays a role in growth-rate in children with limited dietary intake (5). However, the role of zinc in an injury healing context and following athletic injury has not been researched. Nevertheless, even mild insufficiencies in zinc levels could impact the activation of these substances, negatively impact protein turnover and potentially impact the healing and recovery process.
Vitamin D: may help tendon recovery. Since vitamin D plays a key role in bone growth and differentiation, and muscle strength, it may play a significant role in the tendon-to-bone healing process by increasing bone density and strengthening the skeletal muscles. A study concluded that vitamin D3 successfully influences bone and muscle healing, increasing the chances of a tendon-bone repair (6)./p>
Research also shows that supplementation with vitamin D3 is significantly associated with better grip strength recovery at 6 months post injury (7).
Calcium: is essential for good bone health and therefore should be considered of importance in athletic injury prevention and recovery. Research on athletes and calcium intake is limited – however a study on female runners showed an association between increased calcium intake, increased bone density and reduced incidence of stress fractures (8).
Additionally, a study on older adults with hip fractures showed that a specific combined supplementation of CaHMB (a specific type of calcium), vitamin D and protein led to accelerated wound healing, shortening of immobilisation period and increased muscle strength (9).
The following nutrients are indicated to play a role in tendon & ligament health and recovery, however the research to support their role in enhancing recovery or aiding prevention of injury is limited and therefore firm conclusions cannot be drawn.
Vitamin C: is associated with hydroxyproline synthesis, necessary for collagen formation and therefore recognised as being essential for tendon health. However, although a certain level (sufficient levels) is required for collagen synthesis, currently there is no evidence that increasing vitamin C intake will increase collagen synthesis and either prevent injuries or further enhance recovery rates.
Copper: similarly to vitamin C, plays a role in the collagen-containing tissues such as bone. There is no research to suggest an increase in collagen function with increasing doses of copper.
Gelatine/hydrolysed collagen: there is some research to indicate that gelatine or hydrolysed collagen may increase collagen synthesis and potentially decrease injury rates and aid recovery rates in athletes (10).
Curcumin: an anti-oxidant rather than a nutrient, has research to support its role in potentially treating and preventing inflammatory related disorders (11). Supplementation with curcumin has been associated with reduced joint pain, improved mobility and reduced inflammation (12).
A combination of substances known as nutraceuticals, such as curcumin, glucosamine and chondroitin sulfate are indicated to have a beneficial effect on collagen synthesis and inflammation. However, the methodology of these studies is highly questionable and further research is required to determine whether this is the case.
Therefore, whilst deficiencies of micronutrients should be avoided, there is not clear evidence to support higher intakes of these micronutrients during recovery from injury. However, individual variation for sufficient intake of micronutrients should be taken into consideration, along for the potential for athletes requiring higher intakes – depending upon the individual and their status.
Sometimes the questions you must ask are, can this treatment potentially help? Is there any evidence it can do harm or have a negative impact on recovery? As Nutritionists who support injury recovery, we have to consider the potential risk/reward with the recommendations we make. If there is zero risk and potential reward, then you do on occasions have to look beyond only the well excepted research and push the boundaries to other areas that can be optimised. We deal with athletes, stunt performers, actors and more looking to do whatever they can help aid connective tissue recovery, reduce injury risk and accelerate results because how effectively they heal impacts their day-to-day life and employment.
Can specific nutrients support bone repair?
If you’re interested in supporting your bone health to prevent and treat injuries, consider the following key nutrients.
Collagen: known as the glue for connective tissue, plays a vital role in most connective tissue. Collagen may improve bone density (21), joint stability (22), dry skin and brittle hair/nails (23) and reduce joint pain (24).
Calcium: known for its role in healthy bones and teeth, but also important for blood clotting, and muscle and nerve function. Insufficient intake of calcium may deplete levels in the bone and impact bone health. Increasing calcium intake appropriately when need be, may increase bone density (25).
Vitamin D: is necessary for calcium absorption and helps the bone retain the calcium and phosphorus necessary for bone health. Low vitamin D levels are associated with increased fracture rate and therefore increasing vitamin D intake may help prevent fractures (26). Vitamin D may also help muscle strength (27). Vitamin D insufficiency is also very widespread within athletes, especially during the winter months in the northern hemispheres.
Magnesium: is involved in a variety of processes for optimal function of connective tissue. It’s essential for strong bones, as well as healthy muscle and nerve function. Research shows a significant association between magnesium and bone health (28).
Phosphorus: plays multiple roles in the health of connective tissue – think bones, teeth and the health of the building blocks of every tissue (cells). If the diet lacks too little or too much phosphorus is absorbed, the bones may release its stores of phosphorus into the blood, depleting levels necessary for bone health. Research indicates that phosphorus additives, mainly found in fizzy drinks and salad dressings and other processed foods, are associated with negative effects on bone health (29).
Potassium: is important for muscles as well as the maintenance of fluid levels. Food rich in potassium (bananas and avocados) can help neutralise acids in the body and may protect the bone. A high potassium intake from fruits and vegetables may reduce markers that are associated with reduced bone density (29).
Sodium: whilst enough sodium is necessary for the muscles and water balance, too much can cause calcium losses which may impact bone health. Research indicates that reducing sodium intake may therefore be beneficial for bone health (30).
Nitrates: can be converted into nitric oxide substances which play a diverse role in bone health, as well as relaxing arteriole tissues.
Vitamin K: necessary to help the calcium bind to the bone to build the bone.
Additionally, other nutrients such as manganese, copper, boron, iron, zinc, vitamin A and B vitamins can support bone tissue health.
Therefore, consuming a varied diet that is inclusive of dairy, fruits, and vegetables, including the green leafy kind, are likely to be useful sources of the main nutrients that support bone health.
Can specific nutrients support muscle injury recovery?
Vitamin D: vitamin D deficiencies may impair muscle regeneration (13). Vitamin D is also indicated to be important for muscle strength. Therefore, sufficient levels of vitamin D3 may be key for optimising muscle injury recovery.
Polyphenols: are indicated to improve rate of muscle function recovery after damage, as well as reduce muscle soreness and inflammation (14).
Creatine: supplementation has been shown to reduce loss of strength and mass during immobilisation (3).
What foods can help connective tissue health and injury recovery?
Whilst there is little research on the role of micronutrients in the recovery of connective tissue, it is logical to consider the intake of those that play a key role in the growth, maintenance and health of connective tissue. For example, zinc status is integral to protein turnover. Additionally, research does indicate the role of vitamin D in recovery and healing of tendons/ligaments, as well as muscle strength and bone density, as well as there being evidence for the role of calcium – therefore if you are an athlete or in a period of recovery, you may well wish to consider making dietary modifications to improve intake of foods high in these nutrients, alongside potential supplementation.
Here are some other foods that you can’t go wrong including:
Cruciferous vegetables: mustard greens, kale, watercress, Brussel sprouts, cauliflower, broccoli, purple cabbage, bok choy.
Vitamin C rich fruit: strawberries, kiwi, papaya, mango, oranges and grapefruit.
Berries: rich in a variety of nutrients, as well as substances called polyphenols which encourage your body to produce more nitric oxide and aid levels of inflammation.
Bone broth: for your collagen, calcium, magnesium, potassium, phosphorus, sodium and gelatin.
Dark chocolate: is a source of magnesium and copper as well as substances called polyphenols which encourage your body to produce more nitric oxide.
Brown rice, oatmeal and potatoes: rich in fibre to support a healthy gut and levels of inflammation, also sources of calcium, magnesium, phosphorus and great for energy availability.
Green tea: high in the health promoting substance polyphenols, important for a variety of factors – collagen and nitric oxide production, as well as levels of inflammation.
What foods may negatively affect connective tissue health and recovery?
Keep fizzy drinks at a minimum to avoid too much phosphorus.
Limit processed foods to <20% because they have a higher risk of contributing to inflammation in the body. Reducing intake of proinflammatory fat sources (omega 6 fats) such as margarine and vegetable oils. Instead replace with monounsaturated sources of fat, such as olive oil and avocado, as well as omega 3 fats found in oily fish.
Testing nutrient status for connective tissue health
As you can see from the content above, nutrients can play a role in supporting connective tissue health and recovery.
As clinicians, we often run blood and urine-based assessments to look for nutritional insufficiencies in micronutrients, amino acids and fatty acids. We address these insufficiencies not only for general health purposes but also to accelerate recovery and repair from exercise induced injury and general injury from non-exercise activities.
Lifestyle tips to optimise connective tissue health:
Daily 20 minutes of exposure to sunlight: essential for vitamin D production which also drives nitric oxide production, as well as making you feel great so that you can manage life and stress better.
Breathe through your nose: start with once a day for 10 breaths. This optimises nitric oxide production as well as having a calming effect on the nervous system, reducing the stress response and managing inflammatory levels.
Sleep: enough sleep is key for effective management of the stress response. A chronic stress response may be associated with a pro inflammatory response which may be detrimental to the health of connective tissue , as well as impairing the recovery process. Sleep is the time when the recovery processes take place. Enough sleep is also critical for preventing collagen production dropping. Shoot for 7-9 hours per day, waking up at the same time each day.
Exercise: a balance of consistent exercise is important for managing the stress response and reducing levels of inflammation, vital for connective tissue health and recovery. It is also key for maintaining adequate collagen production. If you are injured you may have to adjust your program, however, no matter how injured you are, finding exercise you can and enjoy doing will be crucial for physical and mental well-being.
Manage stress: chronic production of the stress hormone cortisol is associated with a pro inflammatory environment which may impair connective tissue health and recovery, as well as decreased production of collagen. Chronically high cortisol is catabolic, meaning it contributes further to tissue breakdown rather than repair.
Collagen peptides for connective tissue recovery and repair
Collagen peptides are a small digestible form of collagen that may be able to help the body replace lost collagen. Studies have associated supplementation of collagen peptides with improved skin elasticity (15,16), as well as decreased joint pain for those with osteoarthritis (17). There is also some indication that peptide supplementation may be associated with certain improvements in muscle strength and recovery markers via managing the inflammatory response (18).
Since collagen comprises 60% of cartilage, the connective tissue that supports the shock of high-impact movements, it is logical that a breakdown in collagen could lead to a loss in cartilage and joint issues. The effectiveness of collagen supplements is unclear – many studies are funded by collagen related companies, communication via labelling lacks detail and research is limited. However, weighing up risk vs reward, it is likely something that you may want to consider to support connective tissue recovery.
Other therapies that have been shown to speed up recovery.
Stem cell therapy: some research indicates that it may hold promise for improving the health of connective tissue (19).
Cryotherapy: may decrease levels of inflammatory, key for recovery (20).
Key takeaways:
Consuming a consistent nutrient dense diet is the cornerstone of connective tissue health: achieved by following a whole foods diet > 80% of the time and opting for locally grown food, in season where possible.
To enhance the prevention and recovery of connective tissue injury: in addition to consuming a nutrient dense diet, sufficient protein intake, energy intake and overall nutrient sufficiency is key. Omega 3 supplementation may aid levels of inflammation.
Supplementation with vitamin D and calcium: has research to support their benefits in the recovery of connective tissue injuries. Zinc is also implied to be important. Also ensure sufficient intake of vitamin C and copper.
Always consider general lifestyle habits to enhance recovery and prevention of injury of connective tissue: and prioritise good quality sleep and low stress.
Personalise you approach: Get the help of a professional to guide your diet and lifestyle behaviours. This can be further guided with specific tests that help to uncover insufficiencies or imbalances in important nutrients that can aid connective tissue recovery and health.
For more information about working with a member of our team on a 1-2-1 basis and booking in a free 15min discovery call, complete our ENQUIRY FORM.
Alternatively, to learn more about how we work and our consultation options, check out our WORK WITH US page.
References
- 1. Calder et al. (2013). Omega 3 polyunsaturated fatty acids and the inflammatory process.
- 2. Tipton et al. (2015). Nutritional support for exercise-induced injuries.
- 3. Johnston et al. (2009). Effect of creatine supplementation during cast-induced immobilisation on the preservation of muscle mass, strength and endurance
- 4. Kogan et al. (2017). Zinc and wound healing: a review of zinc physiology and clinical applications
- 5. Lannotti et al. (2008). Maternal zinc supplements and growth in Peruvian infants.
- 6. Dougherty et al. (2016). Vitamin D and the immunomodulation of rotator cuff injury.
- 7. Lee et al. (2013). Evaluation of vitamin D level and grip strength recovery in women with a distal radius fracture.
- 8. Tenforde et al. (2010). Evaluating the relationship of calcium and vitamin D in the prevention of stress fracture injuries in the young athlete: a review of the literature.
- 9. Eking et al. (2016). Effect of CaHMB, vitamin D and protein supplementation on postoperative immobilisation in malnourished older adult patients with hip fracture: a randomised controlled study
- 10. Shaw et al. (2017). Vitamin C enriched gelatin supplementation before intermittent activity augments collagen synthesis.
- 11. Chen et al. (2016). Curcumin alleviates glucocorticoid-induced osteoporosis through the regulation of the Wnt signalling pathway.
- 12. Chin et al. (2016). The spice for joint inflammation: anti-inflammatory role of curcumin in treating osteoarthritis.
- 13. Owens et al. (2018). Vitamin D and the athlete: current perspectives and new challenges.
- 14. Peeling et al. (2018). Evidence-based supplements for the enhancement of athletic performance.
- 15. Proksch et al. (2014). Oral supplementation of specific collagen peptides has beneficial effects on human skin physiology.
- 16. Kim et al. (2018). Oral intake of low-molecular weight collagen peptide improves hydration, elasticity and wrinkling in human skin: a randomised, double-blind, placebo-controlled study.
- 17. Bello et al. (2006). Collagen hydrosylate for the treatment of osteoarthritis and other joint disorders: a review of the literature.
- 18. Khatri et al. (2021). The effects of collagen peptide supplementation on body composition, collagen synthesis, and recovery from joint injury and exercise: a systematic review.
- 19. Peng et al. (2003). Stem cells in the treatment of muscle and connective tissue disease.
- 20. Diong et al. (2014). Cold water immersion (cryotherapy) for preventing muscle soreness after exercise.
- 21. Konig et al. (2018). Specific collagen peptides improve bone mineral density and bone markers in postmenopausal women – a randomised controlled study.
- 22. Dressler et al. (2018). Improvement of functional ankle properties following supplementation with specific collagen peptides in athletes with chronic ankle instability.
- 23. Franchesca et al. (2019). Oral collagen supplementation: a systematic review of dermatological applications.
- 24. Clark et al. (2008). 24-week study on the use of collagen hydrosylate as a dietary supplement in athletes with activity related joint pain.
- 25. Tai et al. (2015). Calcium intake and bone mineral density: systematic review and meta-analysis
- 26. Bischoff-Ferrari et al. (2009). Prevention of nonvertebral fractures with oral vitamin D and dose dependency: a meta-analysis of randomised controlled trials.
- 27. Bischoff-Ferrari et al. (2004). Effect of vitamin D on falls: a meta-analysis.
- 28. Farsinjad-Marj et al. (2016). Dietary magnesium intake, bone mineral density and risk of fracture: a systematic review and meta-analysis.
- 29. Vorland et al. (2017). Effects of excessive dietary phosphorus intake on bone health.
- 30. Lin et al. (2003). The DASH diet and sodium reduction improve markers of bone turnover and calcium metabolism in adults.